A 55 yr old female with Fever and Vomitings
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welc
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
55 yr old female farmer by occupation came to opd with chief complaints of
Fever since 5days
Vomitings since 2 days
History of presenting illness:
Patient was apparantly asymptomatic 20 yrs back then she was diagnosed with hypertension and diabetes on regular checkup.
Since 2 yrs she started developing tingling sensation in both lower limbs.
No history of loss of sensation.
No history of numbness, swelling,joint deformity and pedal edema.
Thereafter 5 days ago she developed fever which is of high grade, intermittent which is associated with chills and rigor and relieved on taking medication.It is not associated with cough ,cold sore throat,shortness of breath and palpitations.
No history of diurnal variation.
After 3 days she started vomiting (more than 5episodes) which is non projectile,non bilious, non blood stained and contents are food particles.
No history of abdominal pain and no passage of stools( due to decreased appetite) , flatulence is passed.No history of blood in stools,No history of hemetemesis, No history of burning micturition.
There was history of headache which of severe type present on temporal and parietal region.No history of photophobia and phonophobia.
History of generalized weakness
Past history:
Known case of diabetes and hypertension since 20 yrs
Not a known case of TB, Epilepsy,Asthma,CAD , thyroid disorders
History of previous surgery for renal calculi (25mm)7 yrs back
History of previous cataract surgery in left eye 6 months back
Personal history:
Diet : mixed
Appetite: decreased since 5days
Sleep : disturbed
Bowel and bladder movements: previously regular.No passage of stools since 5 Days
No addictions
No drug or food allergies
Family history : No significant family history
Treatment history:
For diabetes(OHA- Metformin and MIXTARD insulin)
For hypertension (Tab Amlong + Atenolol)
General examination:
Patient is concious ,coherent and cooperative
Moderately built and nourished
Vitals:
Temp: afebrile
PR: 74bpm
RR: 18cpm
Bp: 140/80 mmHg
GRBS: 283mg/dl
No Pallor,Icterus,Cyanosis,Clubbing , Lymphadenopathy,Edema.
Systemic Examination:
CNS Examination:
Higher mental functions:
Patient is conscious,coherent,cooperative,
Speech and language is normal
Memory is intact
No delusions or hallucinations
Cranial nerves:Intact
Olfactory nerve
Optic nerve
Occulomotor nerve
Trochlear nerve
Trigeminal nerve
Abducens nerve
Facial nerve
Vestibulocochlear nerve
Glossopharyngeal nerve
Vagus nerve
Spinal accessory nerve
Hypoglossal nerve
Motor system:
Right Left
Bulk UL n n
LL n n
Tone UL n n
LL n n
Power UL 5/5 5/5
LL 5/5 5/5
Reflexes:
Superficial reflexes: present
Corneal
Conjunctival
Abdominal
Plantar reflexes
Deep reflexes:Present
Right Left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee + +
Ankle + +
Co ordination present
Gait normal
No involuntary movements
Sensory system:-
Spinothalamic:
Rt Lt
Crude touch N N
Pain N N
Temperature N N
Dorsal column:
Fine touch N N
Joint proprioception N N
Rombergs test.
Vibrations: (in seconds)
Acromian process. 7.4 7.7
Olecronon process. 8.5 8.3
Styloid process. 8.0. 8.2
Tibial tuberosity. 5.6 6.0
Shaft of tibia. 3.5. 4
Medial malleolus. 3.5. 4
Cortical:
Graphesthesia. N N
Stereognosis. N N
Romberg's test
Cerebellar signs:
No nystagmus,Finger nose test positive,Heel knee test positive
No signs of meningeal irritation.
CVS Examination:
JVP- Not raised,normal wave pattern.
On inspection:
shape of chest wall elliptical, no visible pulsations, no engorged veins present.
Apical impulse is not visible
Palpation:
apex beat over left 5th intercostal space medial to midclavicular line. No parasternal heaves
No precordial thrill
No dilated veins
Auscultation: S1 and S2 heard no murmurs heard.
Respiratory system:
Chest shape normal
Trachea central
Bilateral air entry Present
Normal vesicular breath sounds
Per Abdomen :
Soft and non tender
No organomegaly
Bowel sounds heard
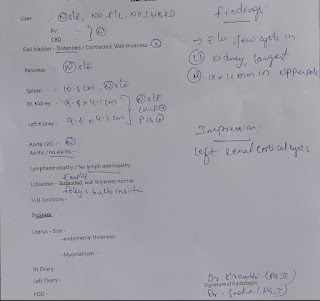
Investigations:
Provisional diagnosis:
Viral pyrexia with uncontolled diabetes( bilateral sensory neuropathy in both lower limbs- stocking type)












Comments
Post a Comment