58 yr old male patient with Shortness of breath , Sweating and fever.
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
58 yr old male patient was admitted with chief complaints of Shortness of breath , Sweating , fever.
HOPI :-
Sequence of events:-
Patient was apparently asymptomatic 7 yrs back then he went to checkup for fever then was diagnosed as Diabetic and aslo with hypotension and was taking medications since then.
Then after 2 yrs he developed ulcers on both the legs after an injury during the field work and there was skin peeling also.
Thereafter he was on a diet for 4 months {which includes drinking organic coconut oil,taking only liquid foods, Vegetables that made him lose his weight (100 to 75 kg)} was healthy but he developed skin infections (fungal) on the lower abdomen and legs and was on medications.
After a year he developed muscle spasm in the left leg and back pain for which he took various unprescribed painkillers (for 2yrs).he also went for physiotherapy 5-6 months back.
3 months back he met with an RTA and had an left ankle injury which was non healing even on medication.
Patient was alcoholic at the age of 15-30 yrs and stopped drinking thereafter.
8 yrs back he again started drinking alcohol due to depression after his son died and stopped when he developed leg ulcers(5 yrs back).
1yr back he consumed alcohol 2-3 times and stopped.
5 days back he started consuming toddy ( after dinner) daily for 3 days.First 2 days he was normal but on the 3rd day before going to sleep at night he started having shortness of breath ( grade 4 ), Sweating, fever and gas trouble.
He was treated by private practitioner on the same night but his condition was not improving so was shifted to the hospital.
Past history:
K/c/o Diabetes and hypotension
Not a k/c/o Asthma,TB, Thyroid disorders, Epilepsy
Personal history:
Diet:mixed
Appetite: Normal
Sleep: adequate
Bowel and bladder movements: regular
Family history: No significant family history
GENERAL EXAMINATION:-
Patient is conscious coherent and cooperative
Well oriented to time place and person
No Pallor, icterus, Cyanosis,Clubbing, Lymphadenopathy
Bilateral Edema is seen from thigh to toes (left more than right)
Vitals:-
Temp: afebrile at the time of examination
HR:112 bpm
BP:80/50
RR: 36 cpm
SYSTEMIC EXAMINATION:
Cvs: s1 s2 heard no murmurs
Respiratory:
Dyspnea is present
NVBS , Bilateral air entry seen
CNS: conscious
Normal speech
No focal neurological deficit.
Per abdomen:
Abdomen is obese and distended, soft and non tender.
Clinical pictures:
Fever chart:
Investigations:
CBP,RFT,LFT
Provisonal diagnosis
Sepsis secondary to left lower limb cellulitis with metabolic acidosis.
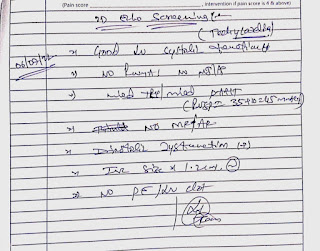
Treatment given on 6/7/22
1.Head end elevation upto 30 degree
2.O2 supplementation if spo2 is less than 90 percentage
3.Inj.PIPTAZ 2.25gm/IV/BD
4.Inj.METROGYL 100ml/IV/BD
5.Inj.HEPARIN 5000IU /IV/TID
6.Inj.Nor-Adr(2amp in 50ml)
7.Inj.PANTOP 40mg/IV/OD
8.Inj.NEOMOL 100ml (if temp greater than 101 degree Fahrenheit)
9.Inj.ZOFER 4mg /IV/SOS
10.Tab.CHYMORAL FORTE/PO/TID
11.Mgso4+ glycerine dressing daily
12.Foot end elevation
13.Inj.HAI /SC/ premeal(8am-2pm-8pm)
14.Monitering vitals hourly
15.Neb-Duolin and Neb -budecort 8th hourly
16.GRBS charting 4th hourly
17.LULICONAZOLE oint
18.IV fluids 100ml/hr


















Comments
Post a Comment