A 40 yr old male with altered sensorium and seizures
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 40 yr old male presented with CHIEF COMPLAINTS of altered sensorium and seizures.
[ ]HOPI:-
Patient was apparently asymptomatic 8 days ago then he developed involuntary movements of both upperlimbs and lower limbs at night.then his wife got a call next day morning saying he is lying on the side a road and brought to casualty.
[ ] PAST HISTORY:-
history of recurrent seizures activity since childhood, first episode occured when he was 5yrs of age when he had fever followed by a seizure episode. he was on medication for 3-4 yrs and discontinued.
h/o alcohol abuse since 20 yrs, started consuming after his sister's death.
he got married thirteen yrs back 2yrs after which he had another episode of seizure at that time alcohol consumption was 90ml/day.
Since 20days he consumed alcohol at 11pm and had seizures 10am the following morning.
His consumption increased over these 20days and decreased food consumption,
last seizure activity was 10 days back.
last binge of alcohol consumption was the day before the seizure.
[ ] PAST HISTORY:-
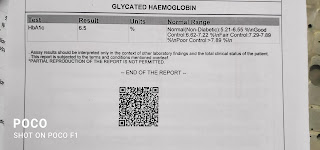
Not an k/c/o HTN, DM, TB, BA, CVA, CAD
[ ] TREATMENT HISTORY:-
no significant past medical and surgical history.
[ ] FAMILY HISTORY:-
no significant family history
ON PRESENTATION
[ ] GENERAL EXAMINATION
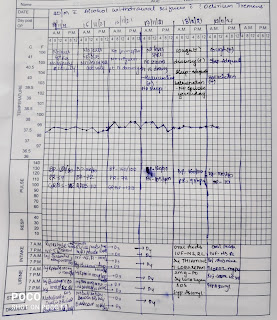
VITALS:-
Afebrile to touch
PR- 58bpm
BP- 110/50
SPO2- 99%
GRBS- 22mg/dl
No pallor ,
No icterus,
No cyanosis,
No clubbing,
No lymphadenopathy,
No edema.
[ ] SYSTEMIC EXAMINATION
CVS- S1 S2+,NO MURMURS.
RS- BAE+ NVBS+
PA- soft, non tender
CNS-
Patient is drowsy
Incoherent speech
No meningeal signs are seen (NECK STIFFNESS,KERNINGS SIGN)
Cranial nerves ,motor system,sensory system couldn't elicit
Gcs- E3,V3,M4.
All reflexes are normal.
Finger nose coordination present
Knee heel coordination present









Comments
Post a Comment